Nutrition and Mental Health
Did your mother ever tell you to “eat right so you can do well in school”? Our moms were smart! What you eat can definitely impact your ability to pay attention, feel more connected and help you think and focus.
You may have forgotten in your adult years to stay connected to your mother’s advice. As you run out the door with a cookie held between your teeth as you fish for your keys and then gulp down a soft drink as you drive, or stop at a drive through for a delicious breakfast sandwich and hash browns, you may have set your body and brain in motion for a quick rush and a hard fall. You may initially feel great, but them fatigue sets in. You find yourself not making the best decisions because you just don’t feel good. Research shows that poor diet not only creates fatigue but can worsen the fatigue that is already associated with levels of stress, anxiety and depression.
Back to your mother; she also probably told you to eat your fruits and vegetables. Again, she was right. Much of what we eat and especially eat when we are on the run, are foods that are processed. We have learned that processed foods operate as addictive substances, stimulating dopamine; accessing the reward centers of our brain. Our brain then tells us that fast foods… processed foods are, oh so crave-able! Just like your mother told you, if you stop eating these foods, you’ll feel better both emotionally and physically.
The American Dietetic Association has discussed issue’s related to both processed foods and how our eating changes with our emotions. Just like your mother, they advise a reduction in high sugar and processed food content in your diet. Blamed for inflammation in both your body and brain, processed foods and sugars can exacerbate depression, sleep disorders, anxiety, and mood related disorders. The other worry is those of us who “forget” to eat at work because of busy-ness or stress and then feeling ill, tired, worn out and nonproductive becomes part of a yoyo behavior. You don’t eat, then when you do, you overeat and eat poorly gorging on high calorie “pick me up” foods. Then you feel awful, you don’t eat and… well you can see where this going, and perhaps; you can look back and see where you have already been. And, again, listen to your mother! She knows what’s best.
Now your mom may not have known what it is called, but your mom probably wanted you to be more mindful about how you behave with food and because of food. NEDA, the National Eating Disorders Association, encourages healthful, mindful eating. Journaling helps and lets you see what times are tough for choosing good foods, what habits are not helping and what, in general, you are choosing. It isn’t always easy, but you can get on track with food and getting on track with food can go a long way for both your physical and emotional health.
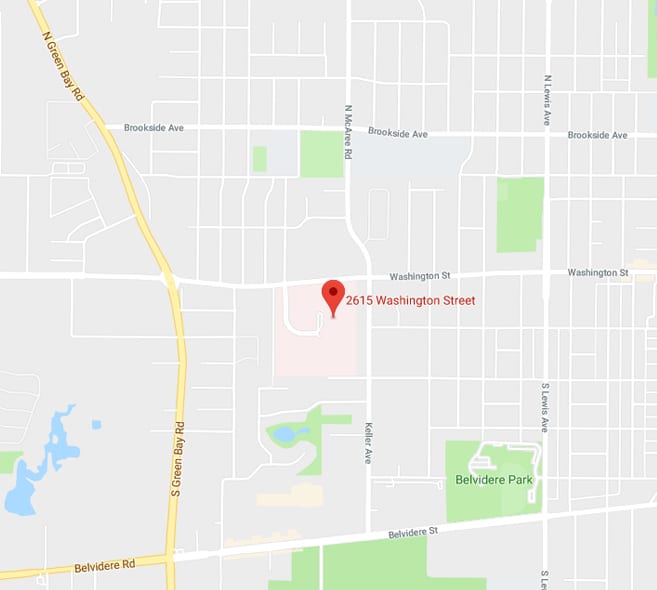
You can’t blame it all on eating though, and when changing your eating to a healthier path doesn’t seem to make you feel any better emotionally; you still feel blue, anxious or sad, it might be time to consider other levels of support. If you are finding that as much as you try, you just don’t feel emotionally better, please call 855-990-1900, and let the caring team at Lake Behavioral Hospital provide a free, confidential assessment that will give you an idea of what level of care is just right for you right now.
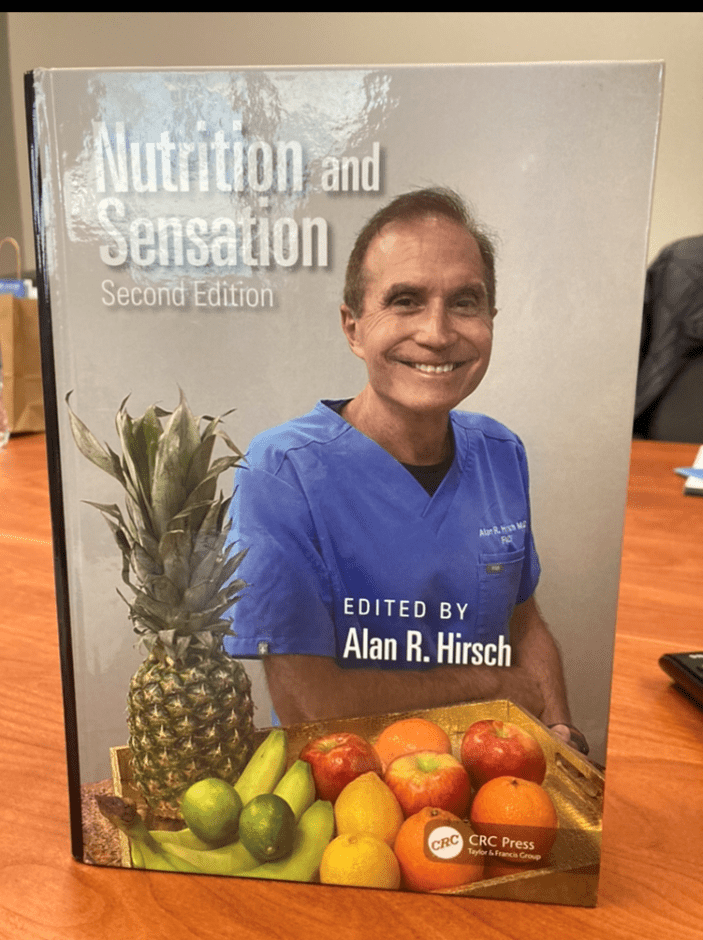
Lake Behavioral Hospital’s own Dr. Alan Hirsch has published the second edition of Nutrition and Sensation. His book explores how the senses influence food’s impact on us. It is fascinating to learn that our senses “fuel consumption” can cause us to experience food in so many ways. From overeating, to obesity and everything in between, Dr. Hirsch’s book really helps the reader understand appetite and, eating and how the influence of food is everywhere.